# Exploring the Benefits of Leech Treatment for Blood and Lymphatic Diseases Understanding Blood and Lymphatic Diseases Blood and lymphatic diseases encompass a wide range of disorders that affect the circulatory and immune systems. These conditions can range from relatively benign issues such as minor clotting disorders to more severe problems like leukemia or lymphoma. Blood diseases often involve the red and white blood cells, platelets, and plasma, while lymphatic diseases primarily affect the lymph nodes and vessels, essential components of the immune system. Common blood disorders include anemia, hemophilia, and clotting disorders, all of which impair the body’s ability to transport oxygen or manage bleeding. On the other hand, lymphatic diseases like lymphedema and lymphatic obstruction can lead to swelling, discomfort, and increased risk of infection. Both blood and lymphatic diseases require careful management to prevent complications and improve quality of life. Treatments for these conditions are varied and depend on the specific disease. They can include medication, lifestyle changes, or more invasive procedures such as surgery or chemotherapy. However, alternative treatments like leech therapy are gaining attention for their potential benefits in managing these conditions. The Historical Use of Leeches in Medicine Leeches have been used in medicine for thousands of years, dating back to ancient Egyptian and Greek civilizations. Historically, leech therapy, or hirudotherapy, was employed to treat a variety of ailments, often based on the belief that it could balance the body’s humors, a foundational concept in ancient medicine. The practice involved placing leeches on the skin to draw blood, thought to cleanse the body of impurities. During the 19th century, leech therapy saw a decline as medical science advanced and new treatments emerged. However, leeches never completely vanished from medical practice. They found a niche role in the treatment of specific conditions, particularly those related to blood flow and clotting. Surgeons also began to recognize their potential in microsurgery, where leeches could enhance circulation and promote healing. In recent years, there has been a resurgence in the use of leeches, driven by a renewed interest in alternative medicine and the discovery of bioactive compounds in leech saliva. These compounds have been found to have anticoagulant, anti-inflammatory, and vasodilatory properties, making leech therapy an intriguing option for managing certain health issues, including blood and lymphatic diseases. How Leech Treatment Works Leech therapy involves the application of medicinal leeches, typically Hirudo medicinalis, to the skin. These leeches attach themselves and begin to draw blood, a process that can last from 20 minutes to an hour. During this time, the leeches release a cocktail of beneficial substances into the bloodstream, which are responsible for the therapeutic effects of the treatment. One of the primary components of leech saliva is hirudin, a powerful anticoagulant that prevents blood from clotting. This allows for improved blood flow and can help dissolve existing clots, reducing the risk of complications from conditions like deep vein thrombosis or stroke. Additionally, leech saliva contains anti-inflammatory agents and vasodilators, which can help reduce swelling and enhance circulation. The effects of leech therapy extend beyond the immediate application. After the leeches are removed, the tiny wounds continue to bleed for several hours, promoting further blood flow and the removal of toxins and excess fluid. This post-treatment bleeding is a critical aspect of the therapy, contributing to its effectiveness in managing blood and lymphatic disorders. Benefits of Leech Therapy for Blood and Lymphatic Diseases Leech therapy offers several potential benefits for individuals suffering from blood and lymphatic diseases. These benefits are largely attributed to the unique properties of leech saliva, which can have significant therapeutic effects on the body. Improved Blood Circulation: By preventing clot formation and enhancing blood flow, leech therapy can help manage conditions that involve poor circulation, such as varicose veins and thrombotic disorders. Enhanced circulation can contribute to faster healing and reduced pain and discomfort. Anti-Inflammatory Effects: The anti-inflammatory compounds in leech saliva can help alleviate symptoms associated with inflammatory conditions, such as arthritis or lymphatic disorders like lymphedema. This can lead to reduced swelling and increased mobility for patients. Pain Relief: Leech saliva contains substances that can act as natural anesthetics, providing pain relief during and after treatment. This can be particularly beneficial for patients suffering from chronic pain due to underlying blood or lymphatic conditions. The combination of these benefits makes leech therapy an attractive option for managing various blood and lymphatic diseases. As with any treatment, it is essential for patients to consult with healthcare professionals to determine if leech therapy is suitable for their specific condition. Scientific Evidence Supporting Leech Treatment Numerous studies have been conducted to explore the efficacy of leech therapy in treating blood and lymphatic diseases, with promising results. Research has shown that leech therapy can effectively reduce symptoms and improve outcomes for patients with conditions such as varicose veins, osteoarthritis, and lymphedema. A study published in the journal Phlebology demonstrated that leech therapy significantly improved symptoms in patients with chronic venous insufficiency, a condition characterized by poor blood flow in the veins. The study found that patients experienced decreased pain and swelling, as well as improved skin condition after undergoing leech therapy. In another study, researchers investigated the effects of leech therapy on patients with knee osteoarthritis. The results, published in the journal Annals of the Rheumatic Diseases, indicated that leech therapy provided significant pain relief and improved joint function, comparable to the effects of conventional pain medication. These studies, along with others, provide a growing body of evidence supporting the use of leech therapy as a complementary treatment for blood and lymphatic diseases. However, more research is needed to fully understand the mechanisms involved and to establish standardized protocols for its use. Potential Risks and Side Effects of Leech Therapy While leech therapy offers numerous benefits, it is not without potential risks and side effects. As with any medical treatment, it is essential for patients to be aware of these risks before undergoing therapy. Infection: There is a risk of infection at the site...
What Causes Heart Blockages? Your Complete Guide
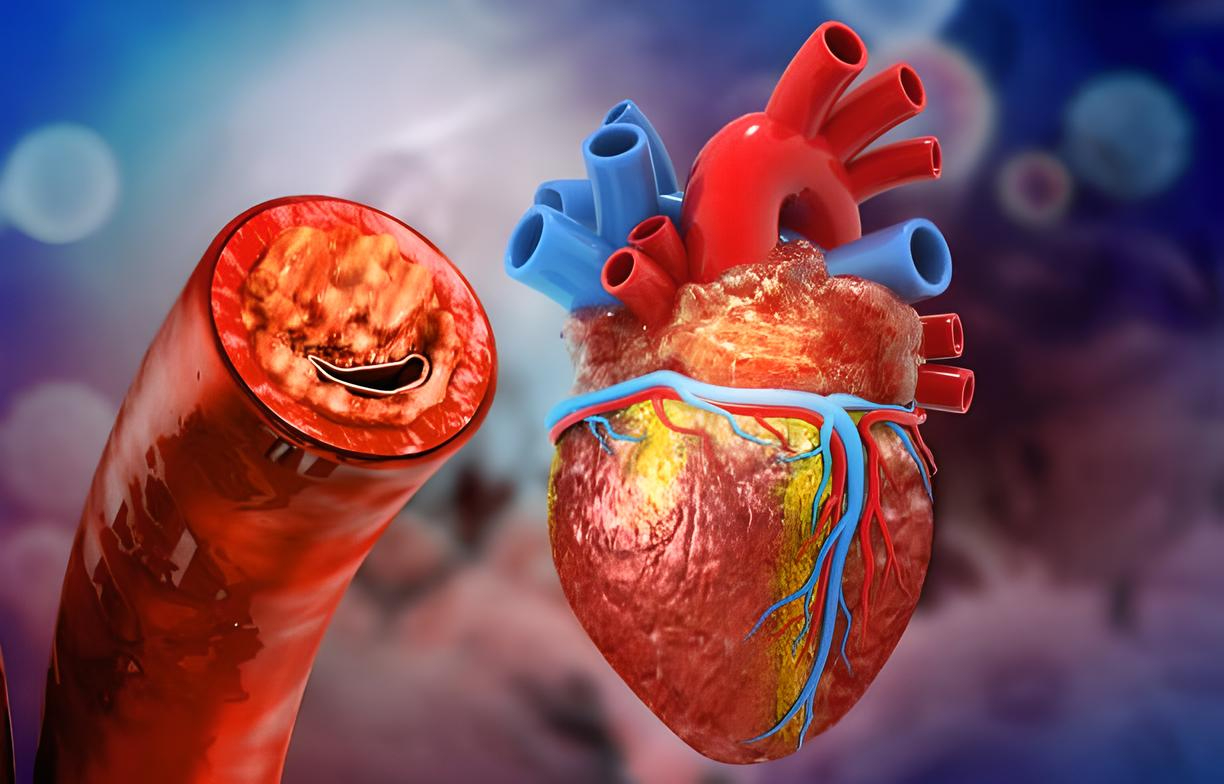
What Causes Heart Blockages? Your Complete Guide The human heart, a remarkable organ that tirelessly pumps blood throughout our bodies, relies on a complex electrical system to maintain its rhythm. When this electrical communication system encounters obstacles, heart blockages can occur, potentially disrupting the heart’s ability to function optimally. Understanding the causes, symptoms, and treatments of these blockages is essential for maintaining cardiovascular health and preventing serious complications. Heart blockages, medically known as atrioventricular (AV) blocks or conduction disorders, occur when electrical signals traveling from the upper chambers (atria) to the lower chambers (ventricles) of the heart encounter interference. This disruption can result in irregular heartbeats, decreased blood flow, and in severe cases, life-threatening conditions. By exploring the intricacies of heart blockages, we can better comprehend their impact on overall health and learn effective strategies for prevention and management. In this comprehensive guide, we’ll delve into the various types of heart blockages, their underlying causes, common symptoms, diagnostic approaches, and treatment options. Whether you’re personally affected by this condition or seeking information for a loved one, this resource aims to provide valuable insights into navigating the complexities of heart blockages with confidence and informed decision-making. Understanding Heart Blockages Heart blockages represent a disruption in the normal electrical conduction system that regulates cardiac rhythm. To comprehend this condition fully, it’s important to first understand how the heart’s electrical system typically functions. The sinoatrial (SA) node, often called the heart’s natural pacemaker, generates electrical impulses that travel through the atria to the atrioventricular (AV) node—a crucial junction that connects the electrical activity between the upper and lower heart chambers. When functioning properly, these electrical signals coordinate the contraction of heart muscles, ensuring blood flows efficiently throughout the body. However, when blockages occur, these signals may be delayed, intermittently disrupted, or completely obstructed, leading to various degrees of heart block. Unlike coronary artery blockages that involve physical obstructions in blood vessels, heart blocks specifically refer to electrical conduction issues that affect the heart’s rhythm and timing. The severity of heart blockages varies significantly, ranging from mild delays in signal transmission to complete interruption of electrical communication between the heart’s chambers. These variations are classified into different types of heart blocks, each with distinct characteristics and implications for heart function. Understanding these classifications helps healthcare providers determine appropriate treatment approaches and management strategies for affected individuals. Heart blockages can develop gradually over time or appear suddenly, depending on the underlying cause. Some individuals may be born with congenital heart block, while others develop the condition later in life due to heart disease, medication effects, or other health factors. The impact on daily life can range from minimal to severe, with some people experiencing no noticeable symptoms while others face significant limitations in physical activity and quality of life. Types of Heart Blockages Heart blockages are categorized into three primary types based on the severity and nature of the electrical signal disruption. First-degree heart block represents the mildest form, characterized by a slowing of electrical impulses as they move through the AV node to reach the ventricles. While the signal eventually reaches its destination, the transmission takes longer than normal. Most individuals with first-degree heart block remain asymptomatic and typically don’t require specific treatment, as the condition rarely progresses to more serious forms without other contributing factors. Second-degree heart block involves a more significant disruption in electrical signal transmission, with some impulses failing to reach the ventricles entirely. This type is further divided into two subtypes: Mobitz Type I (Wenckebach) and Mobitz Type II. In Type I, the electrical signal progressively slows until a heartbeat is completely skipped, creating a pattern of gradually increasing delays followed by a missed beat. This form is generally less concerning than Type II, which involves unpredictable blocking of signals without prior slowing. Mobitz Type II often indicates more serious underlying heart issues and may require intervention with a pacemaker. Third-degree heart block, also known as complete heart block, represents the most severe form of the condition. In this scenario, electrical signals from the atria are completely unable to reach the ventricles, forcing the ventricles to generate their own electrical impulses at a much slower rate. This independent ventricular rhythm is typically insufficient to maintain adequate blood circulation throughout the body, leading to symptoms like fatigue, dizziness, and in severe cases, loss of consciousness. Due to its serious nature, third-degree heart block almost always requires immediate medical intervention, usually in the form of a pacemaker implantation. The progression between these types isn’t always linear, and individuals may experience different forms of heart block at different times depending on underlying causes and overall heart health. Accurate classification is crucial for determining appropriate treatment strategies and monitoring protocols. Healthcare providers use electrocardiograms (ECGs) and other diagnostic tools to identify the specific type of heart block present, allowing for tailored management approaches that address the particular conduction abnormality affecting the patient. Symptoms of Heart Blockages The symptoms of heart blockages can vary dramatically depending on the type and severity of the block, as well as individual factors such as age, overall health, and the presence of other cardiac conditions. In milder forms, particularly first-degree heart block, individuals often remain completely asymptomatic, with the condition only discovered during routine medical examinations or when testing for unrelated issues. This absence of noticeable symptoms can sometimes lead to delayed diagnosis, especially in those who don’t undergo regular cardiac screenings. As the severity increases to second-degree or third-degree heart block, symptoms typically become more pronounced and concerning. Common manifestations include unexplained fatigue that doesn’t improve with rest, shortness of breath even during minimal physical exertion, and lightheadedness or dizziness that may occur suddenly and without warning. Some individuals report experiencing heart palpitations—sensations of fluttering, racing, or irregular heartbeats that can be alarming and disruptive to daily activities. These symptoms often worsen during physical activity when the heart needs to pump more efficiently to meet the body’s increased oxygen demands. More severe symptoms that warrant immediate medical...