What Causes Heart Blockages? Your Complete Guide
What Causes Heart Blockages? Your Complete Guide
The human heart, a remarkable organ that tirelessly pumps blood throughout our bodies, relies on a complex electrical system to maintain its rhythm. When this electrical communication system encounters obstacles, heart blockages can occur, potentially disrupting the heart’s ability to function optimally. Understanding the causes, symptoms, and treatments of these blockages is essential for maintaining cardiovascular health and preventing serious complications.
Heart blockages, medically known as atrioventricular (AV) blocks or conduction disorders, occur when electrical signals traveling from the upper chambers (atria) to the lower chambers (ventricles) of the heart encounter interference. This disruption can result in irregular heartbeats, decreased blood flow, and in severe cases, life-threatening conditions. By exploring the intricacies of heart blockages, we can better comprehend their impact on overall health and learn effective strategies for prevention and management.
In this comprehensive guide, we’ll delve into the various types of heart blockages, their underlying causes, common symptoms, diagnostic approaches, and treatment options. Whether you’re personally affected by this condition or seeking information for a loved one, this resource aims to provide valuable insights into navigating the complexities of heart blockages with confidence and informed decision-making.
Understanding Heart Blockages
Heart blockages represent a disruption in the normal electrical conduction system that regulates cardiac rhythm. To comprehend this condition fully, it’s important to first understand how the heart’s electrical system typically functions. The sinoatrial (SA) node, often called the heart’s natural pacemaker, generates electrical impulses that travel through the atria to the atrioventricular (AV) node—a crucial junction that connects the electrical activity between the upper and lower heart chambers.
When functioning properly, these electrical signals coordinate the contraction of heart muscles, ensuring blood flows efficiently throughout the body. However, when blockages occur, these signals may be delayed, intermittently disrupted, or completely obstructed, leading to various degrees of heart block. Unlike coronary artery blockages that involve physical obstructions in blood vessels, heart blocks specifically refer to electrical conduction issues that affect the heart’s rhythm and timing.
The severity of heart blockages varies significantly, ranging from mild delays in signal transmission to complete interruption of electrical communication between the heart’s chambers. These variations are classified into different types of heart blocks, each with distinct characteristics and implications for heart function. Understanding these classifications helps healthcare providers determine appropriate treatment approaches and management strategies for affected individuals.
Heart blockages can develop gradually over time or appear suddenly, depending on the underlying cause. Some individuals may be born with congenital heart block, while others develop the condition later in life due to heart disease, medication effects, or other health factors. The impact on daily life can range from minimal to severe, with some people experiencing no noticeable symptoms while others face significant limitations in physical activity and quality of life.
Types of Heart Blockages
Heart blockages are categorized into three primary types based on the severity and nature of the electrical signal disruption. First-degree heart block represents the mildest form, characterized by a slowing of electrical impulses as they move through the AV node to reach the ventricles. While the signal eventually reaches its destination, the transmission takes longer than normal. Most individuals with first-degree heart block remain asymptomatic and typically don’t require specific treatment, as the condition rarely progresses to more serious forms without other contributing factors.
Second-degree heart block involves a more significant disruption in electrical signal transmission, with some impulses failing to reach the ventricles entirely. This type is further divided into two subtypes: Mobitz Type I (Wenckebach) and Mobitz Type II. In Type I, the electrical signal progressively slows until a heartbeat is completely skipped, creating a pattern of gradually increasing delays followed by a missed beat. This form is generally less concerning than Type II, which involves unpredictable blocking of signals without prior slowing. Mobitz Type II often indicates more serious underlying heart issues and may require intervention with a pacemaker.
Third-degree heart block, also known as complete heart block, represents the most severe form of the condition. In this scenario, electrical signals from the atria are completely unable to reach the ventricles, forcing the ventricles to generate their own electrical impulses at a much slower rate. This independent ventricular rhythm is typically insufficient to maintain adequate blood circulation throughout the body, leading to symptoms like fatigue, dizziness, and in severe cases, loss of consciousness. Due to its serious nature, third-degree heart block almost always requires immediate medical intervention, usually in the form of a pacemaker implantation.
The progression between these types isn’t always linear, and individuals may experience different forms of heart block at different times depending on underlying causes and overall heart health. Accurate classification is crucial for determining appropriate treatment strategies and monitoring protocols. Healthcare providers use electrocardiograms (ECGs) and other diagnostic tools to identify the specific type of heart block present, allowing for tailored management approaches that address the particular conduction abnormality affecting the patient.
Symptoms of Heart Blockages
The symptoms of heart blockages can vary dramatically depending on the type and severity of the block, as well as individual factors such as age, overall health, and the presence of other cardiac conditions. In milder forms, particularly first-degree heart block, individuals often remain completely asymptomatic, with the condition only discovered during routine medical examinations or when testing for unrelated issues. This absence of noticeable symptoms can sometimes lead to delayed diagnosis, especially in those who don’t undergo regular cardiac screenings.
As the severity increases to second-degree or third-degree heart block, symptoms typically become more pronounced and concerning. Common manifestations include unexplained fatigue that doesn’t improve with rest, shortness of breath even during minimal physical exertion, and lightheadedness or dizziness that may occur suddenly and without warning. Some individuals report experiencing heart palpitations—sensations of fluttering, racing, or irregular heartbeats that can be alarming and disruptive to daily activities. These symptoms often worsen during physical activity when the heart needs to pump more efficiently to meet the body’s increased oxygen demands.
More severe symptoms that warrant immediate medical attention include fainting episodes (syncope), which occur when the heart’s compromised pumping ability leads to insufficient blood flow to the brain. Chest pain or discomfort, though more commonly associated with coronary artery disease, may also manifest in some cases of heart block, particularly when the condition leads to increased strain on the heart muscle. Some individuals experience nausea or excessive sweating alongside other symptoms, especially during episodes of severely compromised heart function.
It’s important to note that symptoms may fluctuate in intensity or appear intermittently, making self-assessment challenging. Some people experience symptom-free periods interspersed with episodes of noticeable cardiac irregularities. Additionally, certain symptoms might be mistakenly attributed to aging, stress, or other health conditions, potentially delaying proper diagnosis and treatment. This variability underscores the importance of seeking professional medical evaluation for any persistent or concerning cardiac symptoms, even if they seem mild or inconsistent.
Causes of Heart Blockages
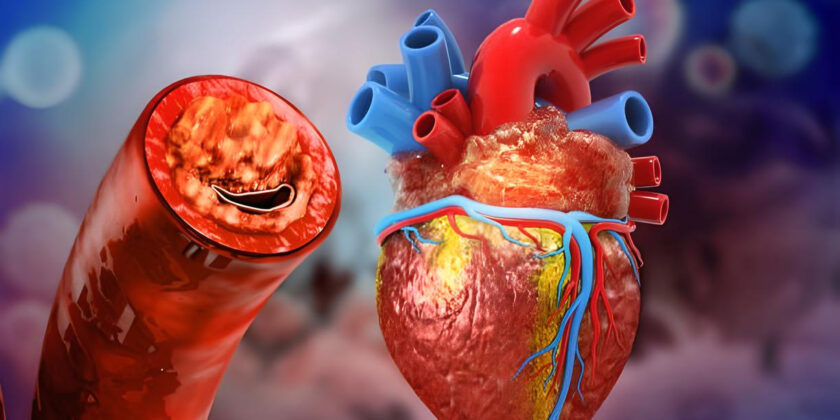
Heart blockages can stem from a diverse range of underlying conditions and factors that affect the heart’s electrical conduction system. Coronary artery disease (CAD) stands as one of the most common contributors, as reduced blood flow to the heart muscle can damage the specialized tissues responsible for electrical signal transmission. When these tissues receive insufficient oxygen and nutrients due to narrowed or blocked coronary arteries, their ability to conduct electrical impulses becomes compromised, potentially leading to various degrees of heart block. This connection highlights the interconnected nature of different cardiovascular conditions and emphasizes the importance of comprehensive cardiac care.
Heart attacks represent another significant cause of heart blockages, as the damage to heart tissue during these events can disrupt the normal pathways for electrical conduction. The scar tissue that forms following a heart attack doesn’t conduct electrical signals effectively, creating potential barriers or delays in the heart’s communication system. The location and extent of the heart attack damage largely determine whether heart block will develop and how severe it might be. In some cases, the blockage may be temporary, resolving as the heart heals, while in others, permanent changes to the conduction system necessitate ongoing management.
Various forms of heart disease that affect the heart muscle itself, collectively known as cardiomyopathies, can lead to heart blockages as they progress. These conditions cause structural changes to the heart muscle that may interfere with normal electrical signal propagation. Similarly, heart valve diseases can indirectly contribute to conduction problems by placing additional strain on the heart chambers or by allowing infections to develop that subsequently affect the conduction system. Congenital heart defects present from birth may also include abnormalities in the development of the electrical conduction pathways, resulting in heart blocks that may be detected in infancy or emerge later in life.
Certain medications, particularly those used to treat other heart conditions, can sometimes cause or exacerbate heart blockages as a side effect. Beta-blockers, calcium channel blockers, and digitalis compounds, while beneficial for many cardiac patients, can slow electrical conduction through the AV node and potentially induce heart block in susceptible individuals. Other potential causes include electrolyte imbalances, particularly abnormal levels of potassium or calcium, which play crucial roles in cardiac electrical activity. Systemic conditions like Lyme disease, sarcoidosis, and certain autoimmune disorders can also affect the heart’s conduction system, highlighting the importance of considering heart blockages within the context of overall health.
Risk Factors for Heart Blockages
Several factors can increase an individual’s susceptibility to developing heart blockages, with advancing age being one of the most significant non-modifiable risk factors. As we grow older, the heart’s electrical conduction system naturally undergoes changes, including fibrosis and calcification of tissues involved in signal transmission. These age-related alterations can impair the efficiency of electrical impulse propagation, making older adults more vulnerable to various forms of heart block. Additionally, the cumulative effects of other risk factors over time contribute to this increased prevalence among seniors, underscoring the importance of regular cardiac monitoring as part of routine healthcare for aging populations.
Family history plays a crucial role in determining risk, as certain types of heart blockages demonstrate genetic patterns of inheritance. Individuals with close relatives who have experienced conduction disorders, particularly at younger ages, may carry genetic predispositions that affect their own cardiac electrical system. These inherited tendencies can manifest as structural abnormalities in conduction pathways or increased susceptibility to factors that damage these pathways. Understanding one’s family cardiac history provides valuable insights for both preventive strategies and diagnostic considerations when symptoms arise.
Pre-existing heart conditions significantly elevate the risk of developing heart blockages, creating a complex interplay of cardiac pathologies that can compound over time. Those with coronary artery disease face increased risk due to potential ischemic damage to conduction tissues, while individuals with heart valve abnormalities may experience conduction disturbances as a secondary effect of their primary valve condition. Heart failure patients often develop electrical conduction issues as their condition progresses, reflecting the interconnected nature of cardiac mechanical and electrical functions. This relationship highlights why comprehensive cardiac care must address both the pumping ability of the heart and its electrical coordination system.
Certain medications, particularly those prescribed for cardiovascular conditions, can increase the likelihood of heart blockages as a side effect. Beta-blockers and calcium channel blockers, while effective for treating hypertension and certain arrhythmias, can slow conduction through the AV node, potentially precipitating heart block in predisposed individuals. Similarly, antiarrhythmic drugs used to manage irregular heartbeats may paradoxically induce conduction abnormalities in some patients. This risk underscores the importance of careful medication management and monitoring, especially in patients with existing conduction system vulnerabilities or those taking multiple cardiac medications simultaneously.
Diagnosis of Heart Blockages
Diagnosing heart blockages typically begins with a comprehensive clinical evaluation that includes a detailed medical history and physical examination. Healthcare providers pay particular attention to symptoms that might indicate compromised heart function, such as unexplained fatigue, dizziness, fainting episodes, or shortness of breath. During the physical examination, the physician listens carefully to heart sounds, noting any irregularities in rhythm or rate that could suggest conduction abnormalities. They may also check for signs of heart failure, such as fluid buildup in the extremities, which can sometimes accompany severe heart blocks. This initial assessment helps guide the selection of appropriate diagnostic tests and establishes a baseline for monitoring the patient’s condition over time.
Electrocardiogram (ECG or EKG) testing serves as the cornerstone of heart block diagnosis, providing a graphical representation of the heart’s electrical activity. This non-invasive test records the timing and strength of electrical signals as they move through different parts of the heart, allowing physicians to identify delays or interruptions in conduction. The characteristic patterns on an ECG can distinguish between first-degree, second-degree, and third-degree heart blocks, each with distinctive features on the tracing. For instance, first-degree heart block appears as a consistently prolonged PR interval, while third-degree heart block shows complete dissociation between atrial and ventricular activities. When heart block is suspected but not captured on a standard ECG, extended monitoring may be necessary.
Ambulatory monitoring devices, such as Holter monitors or event recorders, provide extended ECG recording periods ranging from 24 hours to several weeks. These portable devices allow patients to maintain normal activities while continuously recording their heart’s electrical patterns, increasing the likelihood of capturing intermittent conduction abnormalities that might be missed during a brief standard ECG. Some modern versions even permit remote transmission of data to healthcare providers, enabling real-time analysis and more responsive care. For patients with very infrequent symptoms, implantable loop recorders placed under the skin can monitor heart activity for up to three years, ensuring that even rare episodes of heart block are documented.
Additional diagnostic procedures may include exercise stress testing, which evaluates how the heart’s conduction system responds to increased demands during physical activity. Some heart blocks become more pronounced during exertion, making this a valuable diagnostic tool for cases that aren’t apparent at rest. Electrophysiology studies, though more invasive, provide detailed information about the heart’s electrical system by directly measuring electrical signals through catheters placed inside the heart. This specialized test can precisely locate areas of conduction block and help determine the most appropriate treatment approach, particularly when interventions like pacemaker implantation are being considered. Blood tests may also be performed to identify underlying causes such as electrolyte imbalances or thyroid dysfunction that could be contributing to conduction abnormalities.
Treatment Options for Heart Blockages
The treatment approach for heart blockages varies significantly based on the type and severity of the block, underlying causes, and the patient’s overall health status. For first-degree heart block and some cases of second-degree Mobitz Type I (Wenckebach) block, especially when asymptomatic, careful monitoring without specific intervention may be sufficient. During this watchful waiting period, healthcare providers typically schedule regular follow-up appointments with ECG evaluations to track any progression in the condition. Patients are educated about symptoms that would warrant immediate medical attention, ensuring prompt intervention if the heart block advances to a more serious form. This conservative approach recognizes that milder forms of heart block often remain stable and don’t necessarily progress to more severe types.
Addressing underlying causes represents a crucial component of heart blockage treatment. If the conduction abnormality stems from medication side effects, adjusting dosages or switching to alternative medications may resolve the issue. Similarly, correcting electrolyte imbalances through dietary changes or supplements can improve conduction in cases where abnormal levels of potassium, magnesium, or calcium contribute to the block. When infections like Lyme disease affect the heart’s electrical system, appropriate antibiotic therapy may reverse the conduction disturbance. For heart blocks related to coronary artery disease, treatments aimed at improving blood flow to the heart muscle, such as medications, angioplasty, or bypass surgery, may indirectly benefit the conduction system by enhancing oxygen delivery to specialized conduction tissues.
Temporary pacemakers provide an immediate intervention for patients with symptomatic high-grade heart blocks, particularly in emergency situations. These devices deliver electrical impulses through electrodes typically inserted through a vein and positioned against the heart wall, effectively bypassing the blocked conduction pathway. Temporary pacing may be employed during acute illness, following certain surgical procedures, or while waiting for permanent pacemaker implantation. While effective as a short-term solution, these external pacing systems have limitations, including restricted patient mobility and increased infection risk, making them unsuitable for long-term management of chronic heart blocks.
Permanent pacemaker implantation represents the definitive treatment for most cases of third-degree heart block and symptomatic second-degree heart block. This procedure involves surgically placing a small electronic device under the skin, usually near the collarbone, with one or more leads (thin wires) extending through blood vessels into the heart chambers. The pacemaker continuously monitors the heart’s natural electrical activity and delivers electrical impulses when needed to maintain an appropriate heart rate and rhythm. Modern pacemakers are sophisticated devices that can adjust their pacing rate based on the patient’s activity level, providing more physiological heart rate responses during exercise and rest. Following implantation, patients require regular follow-up appointments for device checks and programming adjustments, ensuring optimal pacemaker function and battery longevity.
Complications of Untreated Heart Blockages
Untreated heart blockages, particularly more severe forms, can lead to a cascade of serious complications that significantly impact both quality of life and long-term survival. Heart failure represents one of the most concerning potential outcomes, developing when the heart’s compromised electrical coordination impairs its ability to pump blood efficiently. The resulting inadequate cardiac output leads to fluid buildup in various body tissues, causing symptoms such as shortness of breath, fatigue, and swelling in the extremities. As heart failure progresses, everyday activities become increasingly difficult, and hospitalization may be required for acute episodes of decompensation. The relationship between heart block and heart failure creates a vicious cycle, as each condition can exacerbate the other, accelerating cardiac deterioration if left unaddressed.
Syncope, or sudden loss of consciousness, poses both immediate safety risks and indicates potentially dangerous underlying cardiac dysfunction. When heart blockages cause the heart to beat too slowly or irregularly, blood flow to the brain may become temporarily insufficient, resulting in fainting episodes that can occur without warning. These events can lead to serious injuries from falls, particularly in older adults, and may precede more catastrophic cardiac events. Recurrent syncope significantly impacts independence and quality of life, as affected individuals may need to restrict activities like driving or living alone due to unpredictable loss of consciousness. The psychological burden of living with this uncertainty often compounds the physical effects of the condition.
Sudden cardiac arrest represents the most devastating potential complication of untreated heart blockages. In severe cases, particularly complete heart block, the heart’s backup pacemaker mechanisms may fail, resulting in prolonged pauses in heartbeat or extremely slow rhythms that cannot sustain life. Without immediate emergency intervention, sudden cardiac arrest rapidly leads to death. Even with prompt resuscitation, neurological damage may occur due to interrupted blood flow to the brain. This risk underscores the importance of timely diagnosis and appropriate management of significant heart blocks, especially in individuals with other cardiac risk factors or previous episodes of concerning symptoms.
Beyond these acute complications, chronic untreated heart blockages can contribute to progressive cardiac remodeling and dysfunction. The heart may enlarge and develop structural changes as it attempts to compensate for inefficient electrical coordination, potentially leading to irreversible damage even if the conduction problem is eventually addressed. Additionally, the reduced cardiac output associated with significant heart blocks can affect multiple organ systems over time, including the kidneys, liver, and brain. This multisystem impact highlights why heart blockages should be viewed not simply as isolated electrical abnormalities but as conditions with potential whole-body consequences that warrant comprehensive medical attention and appropriate intervention.
Living with Heart Blockages
Living successfully with heart blockages often requires thoughtful adaptation to maintain both physical health and emotional well-being. For individuals with pacemakers, understanding device-specific considerations becomes an essential aspect of daily life. While modern pacemakers are designed to be compatible with most everyday activities, certain precautions remain important. Patients should maintain a safe distance from strong electromagnetic fields that could potentially interfere with device function, such as industrial equipment or certain medical procedures. Most household appliances, including microwave ovens and computers, pose no risk when used normally. Carrying a pacemaker identification card and informing healthcare providers about the device before undergoing any medical procedures helps ensure appropriate precautions are taken to protect both the patient and the pacemaker.
Regular medical follow-up plays a crucial role in managing heart blockages effectively, whether treated with a pacemaker or monitored conservatively. These appointments typically include device checks for pacemaker recipients, allowing technicians to verify proper function, optimize settings, and check battery status. For all patients with heart blockages, periodic cardiac evaluations help detect any progression in the condition or development of related cardiovascular issues. Establishing good communication with healthcare providers enables patients to report new or changing symptoms promptly, facilitating timely intervention when needed. This partnership approach to care helps maintain optimal heart function while minimizing the impact of the condition on daily activities and long-term health outcomes.
Adopting heart-healthy lifestyle modifications benefits everyone with cardiac conditions, including those with heart blockages. Regular physical activity, tailored to individual capabilities and medical recommendations, helps maintain cardiovascular fitness and overall well-being. A balanced diet low in sodium and saturated fats supports heart health and helps manage related conditions like hypertension or coronary artery disease that might exacerbate conduction problems. Avoiding tobacco products and limiting alcohol consumption further reduces cardiac strain. For some patients, managing stress through techniques such as mindfulness, meditation, or yoga provides additional cardiovascular benefits by reducing hormonal factors that can negatively impact heart function.
The emotional and psychological aspects of living with heart blockages deserve thoughtful attention, as cardiac conditions often carry significant psychological burden. Many patients experience anxiety about potential symptoms or device malfunction, while others struggle with adjusting to activity limitations or dependency on medical technology. Support groups, either in-person or online, offer valuable opportunities to connect with others facing similar challenges and share coping strategies. Mental health professionals with experience in chronic illness can provide additional support through cognitive-behavioral techniques specifically tailored to address cardiac-related anxiety. Developing a balanced perspective that acknowledges the condition without allowing it to dominate one’s identity helps many patients maintain psychological resilience while living with heart blockages.
Prevention Strategies for Heart Blockages
Preventing heart blockages begins with addressing modifiable cardiovascular risk factors that contribute to heart disease more broadly. Maintaining healthy blood pressure levels stands as a cornerstone of prevention, as hypertension places additional strain on the heart and can damage specialized conduction tissues over time. Regular blood pressure monitoring, medication adherence when prescribed, and lifestyle modifications such as reducing sodium intake and managing stress all contribute to optimal blood pressure control. Similarly, managing cholesterol levels through diet, exercise, and medication when necessary helps prevent the development and progression of coronary artery disease, which can lead to ischemic damage of conduction pathways. These fundamental aspects of cardiovascular health provide protection for the heart’s electrical system alongside their well-established benefits for overall cardiac function.
Regular physical activity offers multiple protective benefits for the heart’s conduction system. Exercise strengthens the heart muscle, improves circulation, helps maintain healthy weight, and contributes to better management of conditions like diabetes that can damage cardiac tissues. The American Heart Association recommends at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous activity weekly, along with muscle-strengthening exercises twice weekly. This balanced approach to physical fitness supports overall cardiovascular health while potentially reducing the risk of developing conduction abnormalities. For those with existing heart conditions, exercise programs should be developed in consultation with healthcare providers to ensure safety and maximize benefits.
Nutritional choices significantly impact heart health and may influence conduction system integrity. A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats provides essential nutrients while limiting substances that contribute to cardiovascular damage. Particular attention to potassium, magnesium, and calcium intake supports proper electrical function in the heart, as these electrolytes play crucial roles in cardiac conduction. Limiting processed foods, which often contain high levels of sodium and unhealthy fats, further protects against conditions that might lead to heart blockages. Some research suggests that anti-inflammatory dietary patterns, such as the Mediterranean diet, may offer additional protection against cardiac electrical abnormalities by reducing systemic inflammation that can affect heart tissues.
Medication management represents an important preventive strategy, particularly for individuals taking drugs that can affect cardiac conduction. Regular medication reviews with healthcare providers help identify potential interactions or side effects that might increase the risk of developing heart blockages. For patients with known conduction system vulnerabilities, careful selection of necessary medications and appropriate dosing can minimize risks while effectively treating other conditions. Additionally, adhering to prescribed treatment regimens for existing cardiovascular conditions helps prevent progression that might eventually affect the heart’s electrical system. This comprehensive approach to medication management acknowledges the complex interplay between various cardiac therapies and their potential impacts on conduction health.
When to Seek Medical Attention
Recognizing situations that warrant immediate medical attention can be lifesaving for individuals with heart blockages or those at risk for developing them. Syncope (fainting) or presyncope (near-fainting) episodes should always prompt urgent medical evaluation, particularly when they occur suddenly or without clear triggers like dehydration or standing up too quickly. These events may indicate periods of insufficient blood flow to the brain due to compromised cardiac function and could signal worsening heart block or other serious cardiac conditions. Similarly, unexplained falls, especially in older adults, should not be dismissed as merely age-related accidents, as they might represent unrecognized syncope episodes resulting from cardiac conduction abnormalities. Prompt medical assessment following these events allows for appropriate diagnostic testing and intervention before more serious complications develop.
Chest discomfort or pain, while classically associated with coronary artery disease, may also occur in some cases of heart block, particularly when the condition leads to heart failure or when it coexists with other cardiac issues. Any new or changing chest symptoms warrant medical evaluation to determine their cause and significance. Shortness of breath that develops or worsens, especially when it occurs during minimal exertion or at rest, could indicate declining cardiac output related to conduction problems and requires prompt assessment. Palpitations—sensations of irregular, racing, or “skipped” heartbeats—might reflect the heart’s attempts to compensate for conduction abnormalities and should be reported to healthcare providers, particularly when they represent a change from previous patterns.
For individuals with implanted pacemakers, certain situations necessitate immediate medical attention. Any symptoms similar to those experienced before pacemaker implantation could indicate device malfunction or battery depletion and should prompt urgent evaluation. Physical trauma to the pacemaker site, even if seemingly minor, requires assessment to ensure the device and leads remain properly positioned and functional. Signs of infection around the implantation site, such as increasing redness, warmth, swelling, or drainage, demand immediate medical attention to prevent the infection from spreading to the bloodstream or heart tissues. Additionally, persistent hiccups or twitching of chest or abdominal muscles might indicate electrical interference with surrounding tissues and warrant prompt evaluation.
Regular communication with healthcare providers about less urgent but still concerning symptoms ensures appropriate monitoring and timely intervention for evolving heart blockages. Increasing fatigue that interferes with daily activities, declining exercise tolerance, or worsening swelling in the legs and ankles should be reported during scheduled appointments or sooner if symptoms progress rapidly. Dizziness that doesn’t result in fainting but occurs regularly, particularly with position changes or exertion, might reflect borderline adequate cardiac output and deserves medical attention. Maintaining an ongoing dialogue about such symptoms helps healthcare providers detect subtle changes in cardiac function that might indicate progression of heart blockages before they result in more serious complications.
Future Directions in Heart Blockage Management
The landscape of heart blockage management continues to evolve with technological innovations that promise improved outcomes and quality of life for affected individuals. Leadless pacemakers represent one of the most significant advancements, eliminating the traditional leads that connect conventional pacemakers to the heart. These self-contained devices, approximately the size of a large vitamin capsule, are delivered directly into the heart chamber through a catheter inserted in the femoral vein. By eliminating leads—the components most vulnerable to complications such as fracture, dislodgement, or infection—these systems potentially offer greater long-term reliability and reduced complication rates. While currently limited primarily to single-chamber pacing, ongoing research aims to expand leadless technology to more complex pacing needs, potentially revolutionizing treatment options for various forms of heart block.
Biological pacing represents an emerging frontier in heart blockage management, focusing on creating biological alternatives to electronic pacemakers. This approach utilizes gene therapy or cell-based techniques to introduce or modify cardiac cells capable of generating spontaneous electrical impulses, essentially creating a biological pacemaker within the heart itself. Research in this area explores various strategies, including reprogramming existing cardiac cells to exhibit pacemaker-like properties or transplanting laboratory-grown pacemaker cells into areas of conduction block. While still primarily in experimental stages, biological pacing holds promise for addressing limitations of electronic devices, such as battery dependency and incompatibility with growing pediatric patients. The potential for a self-sustaining, physiologically responsive system that integrates fully with native heart tissue represents an exciting direction for future treatment paradigms.
Remote monitoring capabilities continue to advance, enhancing the management of patients with heart blockages, particularly those with implanted devices. Modern systems allow continuous or scheduled transmission of device data and relevant physiological parameters directly to healthcare providers without requiring in-person visits. Artificial intelligence algorithms increasingly analyze this data to identify subtle patterns that might predict worsening heart function or device issues before they become clinically apparent. These technologies enable more proactive care models, where interventions can be initiated based on early warning signs rather than waiting for symptom development. As these systems become more sophisticated and integrated with other health monitoring platforms, they promise more personalized and responsive care for individuals with heart conduction disorders.
Precision medicine approaches are increasingly being applied to heart blockage management, recognizing the diverse underlying mechanisms and individual factors that influence both disease progression and treatment response. Genetic testing helps identify specific inherited conduction disorders and guides family screening, while also potentially informing medication choices based on individual genetic profiles. Advanced imaging techniques provide detailed visualization of conduction pathways and areas of block, enabling more targeted interventions. Research into biomarkers specific to conduction system health may eventually allow earlier detection of developing problems before they manifest clinically. This multifaceted approach to personalizing care acknowledges the complex nature of heart blockages and aims to optimize outcomes by tailoring management strategies to each patient’s unique characteristics and needs.
Conclusion
Heart blockages represent a spectrum of conduction abnormalities that can significantly impact cardiac function and overall health. From mild first-degree blocks that may require only monitoring to complete third-degree blocks necessitating immediate intervention, these conditions demand appropriate medical attention and management. Understanding the various types, causes, and symptoms of heart blockages empowers individuals to recognize concerning signs and seek timely care, potentially preventing serious complications like syncope, heart failure, or sudden cardiac arrest.
The diagnostic process for heart blockages has become increasingly sophisticated, with tools ranging from standard electrocardiograms to extended monitoring devices and specialized electrophysiology studies. These capabilities allow for precise characterization of conduction abnormalities, guiding treatment decisions that range from conservative observation to pacemaker implantation. For many patients with significant heart blocks, modern pacemaker technology provides effective management that allows for continued participation in most daily activities with minimal restrictions.
Living successfully with heart blockages often involves a combination of medical management, lifestyle modifications, and regular monitoring. By adopting heart-healthy habits, maintaining open communication with healthcare providers, and following recommended treatment plans, most individuals with heart blockages can maintain good quality of life and overall well-being. The ongoing advances in treatment technologies, from leadless pacemakers to biological pacing research, offer promising directions for even better management options in the future.
Perhaps most importantly, this comprehensive exploration of heart blockages highlights the interconnected nature of the cardiovascular system and the importance of holistic approaches to heart health. By addressing modifiable risk factors, seeking appropriate medical care for concerning symptoms, and engaging actively in treatment decisions, individuals can take meaningful steps toward protecting their heart’s electrical system and ensuring its continued ability to maintain the rhythm of life.